4) Case based OSCE along with Bloom's learning levels acheived .
-September 20 , 2023
Case based OSCE along with bloom’s learning levels achieved.
TODAY’S OSCE:
First we started with IPD cases
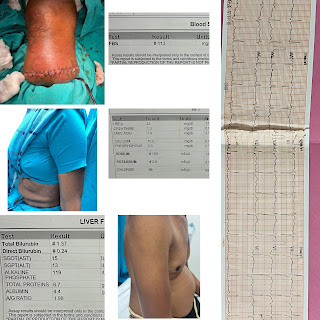
A 71yr old male came to Casuality with chief complaints of decreased urine output since 4months and right lower limb cellulitis and spreading ulcer over right lower limb.
Patient was apparently alright 4months back then he developed decreased urine output.
Patient had history of thorn prick injury on 27/08/23 and has consulted a local RMP for which he had done incision and drainage and then patient developed swelling of right lower limb with boils over right ankle for which he consulted another hospital where they got to know that his creatinine levels are high and patient was referred to KIMS,NKP for hemodialysis.
C/o Fever which is on and off ,high grade,intermittent,associated with chills and rigors.
No c/o polyurea,nocturia,polydypsia
No tingling or burning sensation of b/l upper or lower limbs
No c/o chest pain,palpitations,orthopnea,PND
No abdominal pain,vomiting,loose stools
He was referred to general surgery department I/V/o spreading ulcer over right lower limb ,they diagnosed it as AKI with sepsis with spreading ulcer over right lower limb with DM for which below knee amputation with stump closure under SA was done on 12/09/23
PAST HISTORY:
K/C/O DM since 10 years (on medication)
Not a k/ c /o HTN,thyroid,TB,Epilepsy ,asthma
3sessions of dialysis was done:
16/09/23
17/09/23
19/09/23
2 sessions of PRBC transfusion was done:
17/09/23
19/09/23
PERSONAL HISTORY:
Diet - mixed
Appetite- normal
Sleep - adequate
Micturition:- Normal
Addictions :- alcohol consumption on alternate days since 25yrs (90ml whiskey per day)
Last intake of alcohol is 14days back
GENERAL EXAMINATION:-
Patient is conscious and not oriented to to time and place
No signs of pallor,icterus,cyanosis,clubbing,edema,lymphadenopathy
VITALS:
TEMPERATURE:- 98.8 F
PR:81bpm
BP:90/60mmHg
RR:30cpm
CVS-S1,S2 heard,no murmurs
RS-BAE+,NVBS
P/A- soft,non tender,bowel sounds heard
CNS-NFND
PROVISIONAL DIAGNOSIS:
Chronic kidney disease (diabetic nephropathy) with k/c/o DM 2 since 10yrs
S/P below knee amputation
TREATMENT:
1)IV Fluids
2)Inj.Meropenam 500mg IV / BD
3)Inj.Clindamycin 600mg IV/BD
4)Inj.Lasix 20mg IV/BD (if SBP > 110mmhg)
5)Inj.Neomol 1gm (if temp > 101F)
6)Inj.Human actrapid insulin according to grbs
7)Inj.Noradrenaline (4ml+46ml NS) according to MAP
PaJr group:
https://chat.whatsapp.com/HdKcKlOZiOGHLQgqzxjkxC
QUESTIONS DURING TODAY’S OSCE:
1)Cause of his altered sensorium (delirium)?
Uraemic encephalopathy can be the cause for his delirium
2)Any alcohol withdrawal?what was his alcohol history? Alcohol withdrawal could be the cause of delirium?
He used to consume alcohol every alternate day (90ml whiskey per day) since 25yrs
Last intake of alcohol was 14days ago
So he is in alcohol withdrawal
Delirium is most severe form of alcohol withdrawal
LEVEL 1:
REMEMBERING:
Patient’s history was taken from his attenders and his history and the sequence of events was remembered.
Patient had history of thorn prick injury on 27/08/23 and has consulted a local RMP for which he had done incision and drainage and then patient developed swelling of right lower limb with boils over right ankle for which he consulted another hospital where they got to know that his creatinine levels are high and patient was referred to KIMS,NKP for hemodialysis.
C/o Fever which is on and off ,high grade,intermittent,associated with chills and rigors.
PAST HISTORY:
K/C/O DM since 10 years (on medication)
Not a k/ c /o HTN,thyroid,TB,Epilepsy ,asthma
3sessions of dialysis was done:
16/09/23
17/09/23
19/09/23
2 sessions of PRBC transfusion was done:
17/09/23
19/09/23
LEVEL 2:
UNDERSTANDING:
Understanding the patient’s condition
Initially there was a thorn prick and due to which he developed cellulitis and a spreading ulcer of right lower limb that eventually land up into sepsis.
Sepsis can lead to acute kidney injury by decreasing the GFR.
https://www.nature.com/articles/s41581-023-00683-3/figures/1
He was also on alcohol withdrawal from 14days due to which he developed altered sensorium / delirium.
LEVEL 3:
APPLYING:
Necessary investigations were done and as his s.creatinine was around 4.5 he was kept on maintainance hemodialysis.
Below knee amputation was also done I/V/o spreading ulcer over the right lower limb.
LEVEL 4:
ANALYSIS:
Clinical approach to altered sensorium?
In this patient the cause of his altered sensorium can be metabolic encephalopathy(uraemia) or alcohol withdrawal .
LEVEL 5:
EVALUATING:
List the patient’s problems priority wise—
1)Altered sensorium
2)Hypotension
3)AKI secondary to sepsis for which he was on MHD
Then we were asked to present OPD cases and make their respective PaJr groups -
CASE 1:
A 65yr old male who is a resident of Nalgonda and weaver by occupation came to medicine OPD with complaints of shoulder pain since 1month and lower backache since 1month.
Patient was apparently alright 1month ago then he developed shoulder pain and lower backache which is insidious in onset,gradually progressive in nature.Aggravates on working and relieves by rest.
No c/o chest pain,burning micturition,sweating,fever,cough,cold
K/C/O DM 2 since 4yrs and on metformin 500mg po/od
K/C/O HTN since 4yrs and on Telma 20mg po/od
Daily routine:
Patient works as a weaver.
He wakes up at 5am ,walks for 15-20min has his breakfast at 7am and goes for work by 8am and works till 11am and has his lunch by 12pm rest for an hour and then goes to work by 2pm and works till 4pm ,has his dinner by 7pm and goes to bed by 9pm.
VITALS-
BP-120/70mmhg
PR-78bpm
RR-18cpm
PaJr group:
https://chat.whatsapp.com/JLIhSIeYCpoJZ9pagZ2UZq
CASE 2:
A 40yr old female resident of Nalgonda came to medicine OPD with chief complaints of headache and joint pains since 3days,SOB since 3days.
Patient was apparently alright 3days then she developed headache and joint pains which is pricking type of pain,sudden in onset and non progressive.
H/o Fever since 3days which is sudden in onset,intermittent in nature ,associated with chills and rigors.Relieved by taking medication and no aggrevating factors.Associated with cold and cough.
H/o orthopnea + , SOB aggrevates by taking food
No c/o chest pain,burning micturition,sweating,nausea,vomiting,loose stools
N/K/C/O DM 2,HTN,Asthma,TB,Epilepsy,CVA, CAD
Daily routine:
She is a homemaker
She wakes up at around 6am ,has her breakfast at 7:30 am and does her household chores ,has her lunch at around 12:30 pm and rest for 2hrs,watches TV for sometime and again continue with her household chores,has her dinner at 9pm and goes to bed by 10:30pm.
VITALS:
BP-110/70mmhg
PR-84bpm
RR-18cpm






Comments
Post a Comment