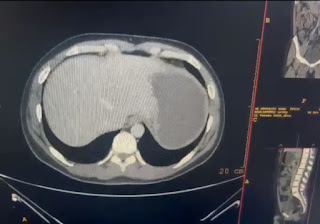
38yrs old male with abdominal pain
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 38 year old male , civil engineer by profession and resident of West Bengal came to OPD with chief complaints of :
Abdominal pain since 5years
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 5 years ago then he developed pain in abdomen which is sudden in onset and progressive in nature.Pain occurs once in a month.Abdominal pain is radiating to the back and dragging type of pain.
Pain aggravates on taking alcohol and relieved by medication.
For the past 1 year patient has episodes of vomiting followed by pain in abdomen ,which is non bilious and water as content.
Associated with weakness and giddiness.
Patient had multiple episodes of vomiting on 13th november ( post lunch) associated with weakness and giddiness ,which didn’t get relieved on medication and had to go to hospital.
From 5years he has abdominal pain occurring once in 3months but from last 6 months he is experiencing pain atleast once in a month.
He also complains of severe weight loss. He was 86 kgs 6 months ago but at present he reduced to 67 kgs.
He also has history of depression for which he is attending psychiatric counselling sessions.
Patient also complains of constipation and per rectal bleeding since childhood.
In his childhood he had trauma to the nose while playing football and developed deviated nasal septum which is not effecting his respiration and his daily activities.
Daily routine: He wakes up at 6am in the morning , gets ready and have breakfast ,go to the office ,completes his work and returns by 5pm and plays badminton or football and then comes to home ,have dinner at 8pm and goes to bed by 10pm.
PAST HISTORY:
Known case of hemarroids from 12yrs of age
Episode of jaundice when he was 12 yrs old
Not a known case of DM, HTN,asthma,TB,epilepsy
History of appendicectomy when he is 17 yrs old
FAMILY HISTORY: No significant family history.
PERSONAL HISTORY:
DIET- Mixed
APPETITE- Normal.
SLEEP- inadequate
BOWEL AND BLADDER MOVEMENTS -
Constipation from 12 years of age (blood stained stools)
Normal bladder movements.
ADDICTIONS-
ALCOHOL- 180 ml every day from 20years .He has stopped consuming alcohol from 6 months because it increases the severity of abdominal pain.
SMOKING- 2 packs a day from when he was in college. 1 pack a day from 6 months.
ALLERGIES- no allergies
GENERAL EXAMINATION:
Patient was conscious , coherent ,cooperative , well oriented to time , place and date.
moderately built and nourished
Vitals:
Temperature - 94*F
PR :- 80 bpm
RR :-16 cpm
BP :- 110/70 mm Hg
SPO2 :- 98%
Pallor: absent
Icterus: absent
Cyanosis: absent
Clubbing: absent
Lymphadenopathy:absent
Pedal edema:Absent
SYSTEMIC EXAMINATION:
CVS-S1, S2 heard,no murmurs
Respiratory System:-
BAE- present
NVBS- heard
Per abdomen:-
soft , non tender.
CNS- no focal deficits



















Comments
Post a Comment